What Is Trauma, Really? (And Why It Matters in Care)
An invitation to understand trauma with compassion and clarity
This is part 1 of our 6-part Trauma-Informed Care Series.
What Is Trauma, Really? (And Why It Matters in Care) (you are here)
The Body Remembers: Trauma and the Nervous System (coming soon)
What Does Trauma-Informed Actually Mean? (coming soon)
Signs of Trauma-Informed Care (What It Looks and Feels Like) (coming soon)
Trauma-Informed Care: Red Flags (coming soon)
The Space Between Us: Shared Responsibility in Trauma-Informed Care (coming soon)
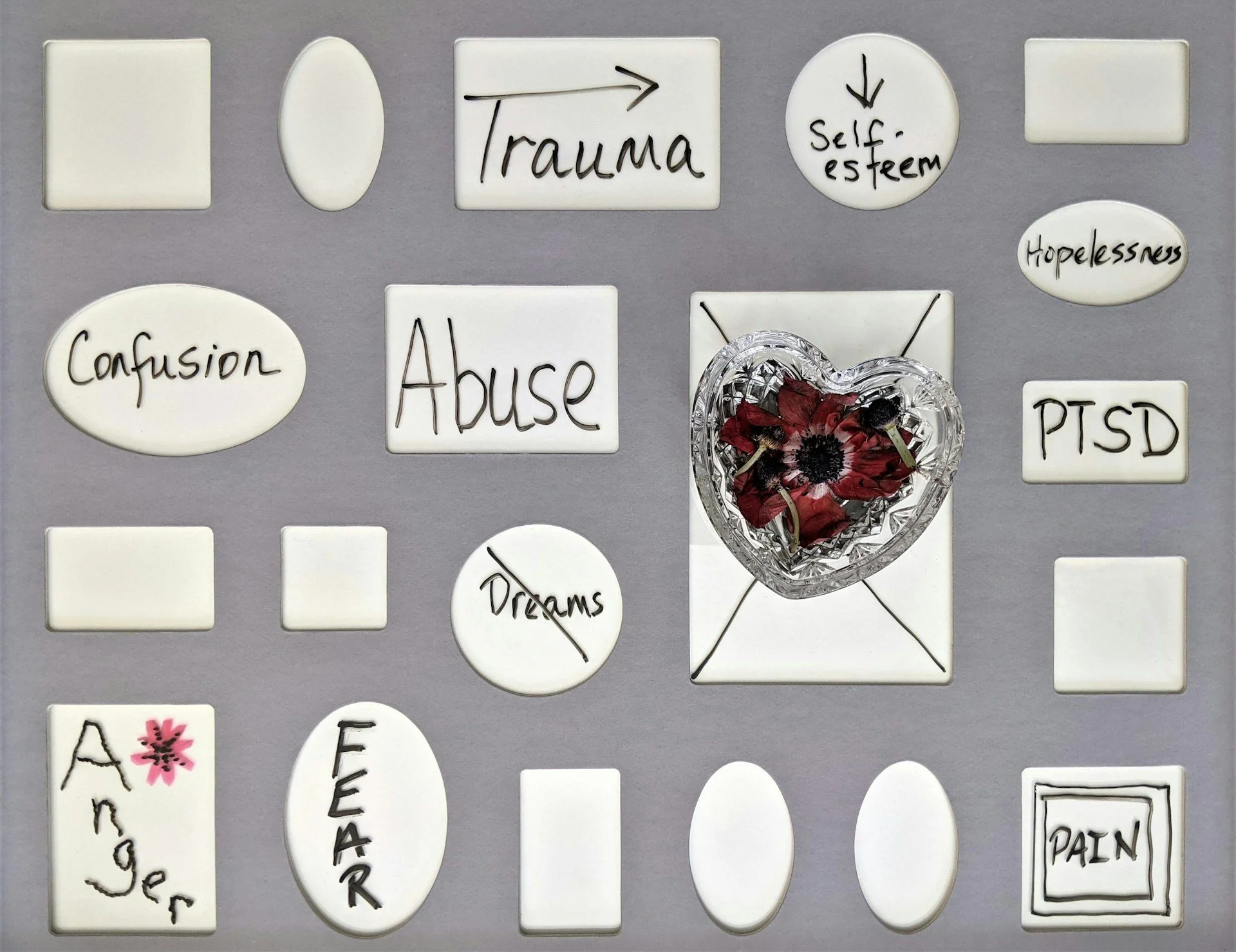
Trauma isn’t just about dramatic events. It’s about how the body and mind respond to what happened (or didn’t happen). This post introduces a grounded, compassionate view of trauma and why it matters in care. We’ll explore how trauma is stored in the body, how it affects daily life, and the Traditional Chinese Medicine (TCM) frameworks that help us understand it.
The Word “Trauma” Is Everywhere Now
From therapy rooms to TikTok, from clinical charts to coffee shop conversations "trauma" is a word that shows up everywhere. It’s good that we’re finally talking about it.
But with all that exposure, the word can start to feel watered down, over-applied, or even incorrectly. So let’s slow things down. Let’s pause and ask:
What is trauma, really?
Is it always tied to a specific event?
And most importantly: why does it matter in care?
This post isn’t a diagnosis checklist. It’s a grounded, heart-forward invitation to explore how trauma shapes our bodies, behaviours, and beliefs, and how compassionate care can help us come home to ourselves again.
Trauma Isn’t the Event. It’s the Response
When most people think of trauma, they picture war zones, car accidents, or abuse.
But here’s the thing: trauma isn’t defined by the event. It’s defined by your body’s response.
“Trauma is not what happens to you. It’s what happens inside you as a result of what happens to you (or didn’t happen).”
—Dr. Gabor Maté
In simpler terms:
Abuse = something happened that shouldn’t have happened.
Neglect = something didn’t happen that should have.
And one of the biggest factors that determines whether something becomes traumatic is this: Did you have support while it happened? Or were you alone?
Trauma Has Many Forms
You might hear terms like:
Acute trauma – a one-time shock
Chronic trauma – ongoing or repeated stress
Complex trauma – especially early, relational trauma
PTSD / C-PTSD – clinical terms with specific criteria
Not everyone who goes through trauma gets diagnosed with PTSD. And not everyone who suffers meets a textbook definition. But that doesn’t make the pain less real.
Feeling Alone Can Be the Wound
Imagine this: You’re a kid, and you’re bullied at school. You come home, and an adult says:
“That must’ve hurt. I’m here for you.” (Cue hug.)
Your pain is seen. Your body settles. You feel held.
Now imagine a different response:
“Toughen up. It’s not a big deal.”
Your nervous system stays revved. You learn to stuff it down.
That’s the seed of trauma. And it’s not always about what happened. It’s about whether someone was there to help you carry it. And that if the experience was well digested or stays in you.
In fact, people who survive natural disasters with others often report less trauma than those who endured quiet, emotional pain in isolation. Why? Because the support system and being witnessed matters. The body regulates better with another nervous system.
Subtle Doesn’t Mean Small
Trauma doesn’t always shout. Sometimes it whispers:
A quiet sense of unworthiness
A habit of over-functioning or perfectionism
Emotional numbness that feels safer than hope
You might forget the moment it began, but your body remembers.
Common Trauma Symptoms
Trauma can show up as:
Insomnia or nightmares
Chronic pain or tight muscles
Digestive problems
Addictions (including overwork or distraction)
People-pleasing, over-controlling, or freezing
Panic attacks or constant low-level anxiety
Shame, hopelessness, or self-blame
And, many people are misdiagnosed with anxiety, depression, ADHD, bipolar disorder, or personality disorders when trauma is underneath it all.
Types of Trauma
Trauma comes in many forms, including:
Big “T” trauma: assault, accidents, disasters
Little “t” trauma: microaggressions, chronic stress, emotional neglect
Sexual trauma
Developmental trauma
Attachment/Relational trauma
Birth & reproductive trauma
Intergenerational trauma
Collective trauma (racism, colonization, displacement)
Vicarious trauma
All of it matters. All of it is valid.
Trauma = Threat Without Support
If you want one line to define trauma, it’s this: A sense of threat (real or perceived) + lack of support.
If someone was there to help you hold it, your body had a chance to process. If not, it got stored. Undigested. Unspoken.
Trauma-Informed Care: Not a Buzzword
Being trauma-informed doesn’t mean treating people like they’re broken. It means recognizing the intelligence of the body’s adaptations.
Trauma-informed care centres on:
Felt safety (not just “safe space” stickers)
Empowerment and choice
Transparency and trust
Respect for culture and lived experience
Listening without judgment
In this kind of care, the goal isn’t to fix. It’s to witness, regulate, and empower.
Why This Matters in Care
Unprocessed trauma can show up in the body in many forms: chronic pain, fatigue, digestive issues, anxiety, autoimmune flares, or dissociation. When healthcare providers don’t understand how trauma shapes the body and mind, well-meaning treatments can fall short or worse, retraumatize.
That’s why trauma-informed care matters. It shifts the question from “What’s wrong with you?” to “What happened to you?” It acknowledges that people may be carrying invisible histories that influence how they relate to their bodies, to providers, and to healing itself.
It also reminds us that healing isn’t just about removing symptoms. It’s about restoring a sense of safety, agency, and connection, on every level.
How Traditional Chinese Medicine (TCM) Understands Trauma
Trauma isn’t new. TCM has mapped how emotional pain lives in the body for centuries:
Kidneys & Heart: Fear disrupts the heart-kidney axis, affecting willpower and spirit.
Sinews (Jing Jin): Muscle tension and defensive postures reflect stored guarding.
Luo Vessels: Hold unresolved emotional experiences.
Divergent Channels: Route trauma deeper when it can’t be processed.
8 Extraordinary Vessels: Store identity-based, ancestral, and developmental trauma.
With acupuncture, herbs lifestyle and dietary work, we help restore what was blocked:
Rebuild sleep, digestion, and emotional resilience
Support the nervous system with gentle regulation
Create space for integration, not just symptom relief
In this blog series, we’ll explore the ripple effects of trauma through the nervous system, what trauma-informed care actually looks and feels like, how to recognize when care isn’t safe (and what to do about it), and why healing isn’t linear.
You don’t need a diagnosis to deserve care that respects your story.
Whether you’ve been navigating trauma for years or just beginning to wonder if your body’s symptoms might be linked to something deeper, this is a place for gentle curiosity, not judgment.
If something here resonates, I hope you’ll read on.