Trauma-Informed Care: Red Flags
How to recognize when care is not truly trauma-informed, and how to trust what your body already knows.
This is part 4 of our 6-part Trauma-Informed Care Series.
Signs of Trauma-Informed Care (What It Looks and Feels Like)
Trauma-Informed Care: Red Flags (you are here)
The Space Between Us: Shared Responsibility in Trauma-Informed Care (coming soon)
Trauma-informed care isn’t about labels, it’s about how care feels. This post outlines how to spot signs of trauma-informed practice, from body language to language tone, and includes questions you can ask when choosing a provider.
What If It Doesn’t Feel Right?
Sometimes the body knows before the mind does. You might leave a session feeling more agitated than before. Maybe there was a vague sense of being rushed or dismissed. You can’t quite explain it, but something felt off.
This post is for those moments. The ones that leave you wondering: Was that actually okay? Is this person really offering trauma-informed care?
Even when a clinic markets itself as “trauma-informed,” that doesn’t guarantee each provider has integrated that framework into how they actually work. Language can be polished. Policies can be well-intentioned. But how you feel in your body, in your nervous system, often tells the real story.
Red Flags in Supposedly Trauma-Informed Care
These signs aren’t about nitpicking or expecting perfection. They’re about helping you stay attuned to your own experience, so you can recognize care that may not be safe or aligned for you.
Dismissiveness or Minimizing Your Experience
If your concerns are waved away or you’re told “everyone feels that way”, that’s a red flag. Trauma-informed care honours your lived experience. It requires curiosity, not assumption. Respect, not deflection.
Rushing Through Sessions
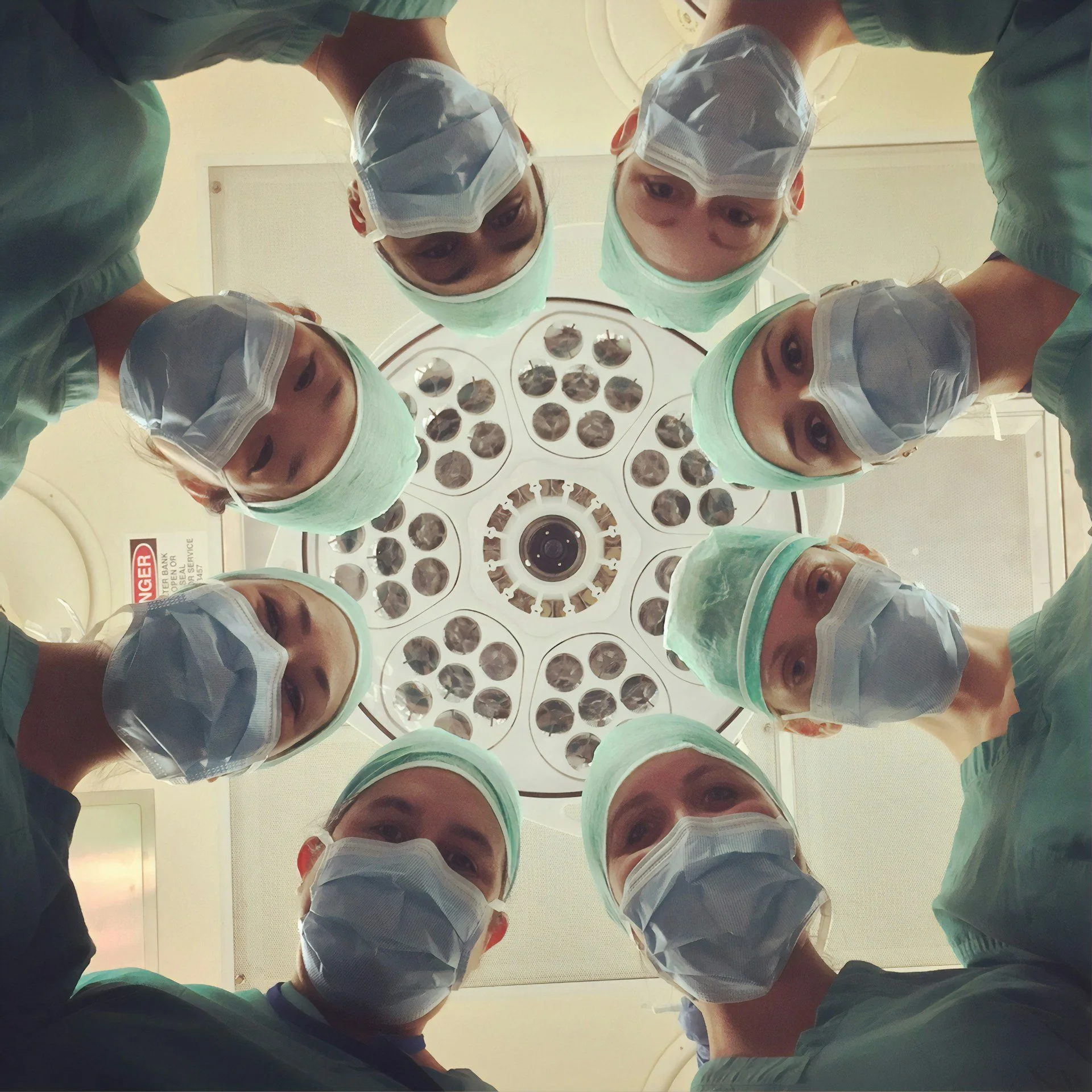
Care shouldn’t feel like a conveyor belt. If you're being hustled through an intake, a procedure, or a conversation, especially if there’s pressure to decide quickly, it may not be trauma-aware care.
Lack of Informed Consent
Consent isn’t just about signing paperwork. It's about being given clear information, having your questions welcomed, and feeling free to say no. If a provider skips explanations or makes you feel guilty for hesitating, that’s not consent, it’s coercion.
Rigid Protocols, No Room for Adaptation
Trauma-informed care is responsive. If there’s no room for feedback, pacing, or adjusting to your capacity, it may replicate the very dynamics that caused harm in the first place.
“Fixing” Mentality or Savior Energy
If a provider positions themselves as the expert who’s going to “fix” you without involving you in decisions that’s not collaboration. It’s hierarchy. Real healing isn’t about being rescued. It’s about being seen, heard, and met where you are.
“My Way or the Highway”
If someone can’t tolerate a “no” or acts offended when you assert a boundary, that’s a problem. Your care is not their performance stage. You don’t owe anyone access to your body or story.
Unregulated Emotional Reactions
A trauma-informed provider does their own work. If they become defensive, triggered, or visibly dysregulated in response to your emotions or limits, they may not be resourced to support you safely.
Blurry Boundaries
Oversharing personal stories, extending sessions unnecessarily, or treating you like a confidante instead of a patient, all of these can signal unclear boundaries. And unclear boundaries often mean the provider is unconsciously trying to meet their own needs through the relationship.
Your Body Is Allowed to Say No
It doesn’t matter how qualified or recommended someone is, if your body says this doesn’t feel right, you’re allowed to listen. You don’t need a perfect explanation to pause or walk away. You don’t owe anyone your continued participation in care that doesn’t feel good.
You can say no. You can take time. You can choose someone else. That is trauma-informed care: choice, voice, and safety.
And If You’re a Provider...
If any of this stings a little, it’s okay. Many of us have had moments we wish we’d shown up differently.
Trauma-informed care isn’t about getting it right all the time. It’s about staying humble, staying curious, and doing the inner work so we can truly be present for the people we serve. We don’t have to be perfect. But we do need to be accountable.
Coming Next: The Space Between Us
In the final post of this series, we’ll reflect on what trauma-informed care really means beyond checklists and buzzwords. We’ll talk about how care providers carry trauma, too, and how healing always happens in relationship. Not to someone, but with them.